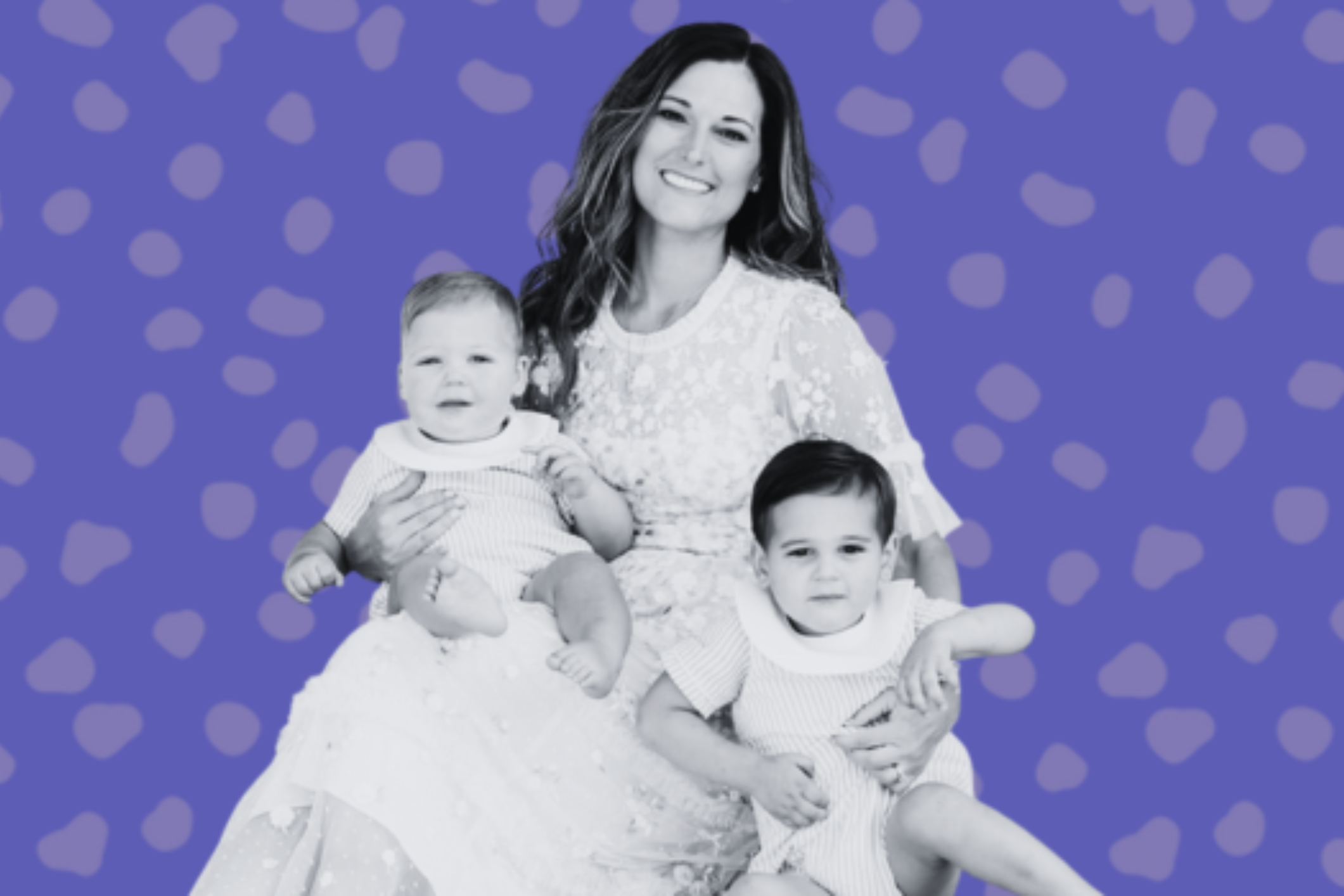
In a recent podcast interview, Paris Hilton, age 39, revealed that she is undergoing IVF “so I can pick twins if I like.” It has also been previously reported that Paris froze her eggs and even went through the process a couple of times.
Regardless of her reasons to do IVF, whether it is to achieve boy/girl twins and/or to address infertility issues she’d rather not share with the public, we know that IVF is not an easy road for anyone.
Her journey through IVF and egg freezing does bring awareness to others who have traveled the same path, and for that, we commend her willingness to be open about her experiences.
Should she succeed in her goal of a twin pregnancy, there will be no misconceptions as to how she achieved this goal, erasing the many questions women commonly have as to how celebrities seem to have infertility unaffected by time.
Paris Hilton’s IVF story also likely brings up some questions for some of you, and we spoke with Dr. Jennifer Hirshfeld-Cytron, Director of the Center for Fertility Preservation, to provide clarity.
Q: Can someone just go to a fertility clinic, undergo IVF, and request boy/girl twins?
A: Yes, but it is extremely rare that someone would undergo the process simply to increase the chances of a specific gender and for a twin pregnancy. IVF is not an easy process and genetic testing would be required to uncover the gender. For many, the costs can be partially or completely out of pocket. This is an unusual situation and should not be considered the norm.
Q: Aren’t twins common with IVF?
A: Twin or multiple pregnancies during IVF have been trending downward for many years. The standard of care is to transfer one embryo with the goal of a healthy singleton pregnancy. In extremely rare cases one embryo can split into twins, but chances of this are <1%. To put this into perspective, your chances of having twins naturally are less than 5%. If two embryos are transferred during IVF, the chances of having twins jumps to 25-40%.
The chances of having twins or a multiple pregnancy can jump even higher if a woman is placed on ovarian stimulation medications such as Clomid, which can cause multiple eggs to be released during ovulation. Close ultrasound monitoring is required when doing a medicated cycle so that a patient is aware that a twin or multiple pregnancy might occur prior to intercourse.
Q: Why is a single embryo transfer the standard of care?
A: As a physician, my goal is to achieve a live birth while also taking into consideration the health of a mother. For these reasons, a singleton pregnancy is always recommended. In cases of advanced maternal age, recurrent pregnancy loss, and a lack of success with prior IVF cycles, two embryos may be recommended.
It’s important to keep in mind that the decision of how many embryos to transfer is ultimately determined by the patient. This is truly a personal decision and we always aim to provide the best guidance possible to help people achieve the goal of a healthy baby and mother.
Q: What are the risks of a twin pregnancy?
A: The idea of twins may sound fun, but a twin pregnancy presents serious risks to both mother and babies. Approximately 60% of twins deliver early. Premature pregnancies increase a child’s risk of impaired lung development, cognitive function and brain development. Twins also have 5x the risk of stillbirth and 7x the risk of neonatal death. Twins born <32 weeks, in particular, have a higher risk of high-grade intraventricular hemorrhage and periventricular leukomalacia that contributes to increased prevalence of cerebral palsy.
Mothers carrying twins have a higher risk of hyperemesis, diabetes, C-section, anemia, hypertension, and a higher likelihood and earlier onset of preeclampsia. Placental abruption increases to 4.7% in twins from 0.7% in singletons. Preterm delivery <35 weeks also occurs in 34.5% of twins vs. 6.3% of singletons.
Q: What needs to be done to uncover the gender of an embryo?
A: Embryo genetic testing, known as preimplantation genetic testing because the testing is done prior to embryo transfer to the uterus where it “implants” and grows, would need to be completed to uncover gender. Traditionally, preimplantation genetic testing is done to identify any genetic abnormalities, whether that is for a known genetic disease in the family or the parents being genetic carriers of a genetic disease. In the case of gender, some genetic issues can only be passed along in a female or male, which is why gender can be an important consideration during family planning.
Q: What are the chances of success for a twin pregnancy at age 39?
A: The general odds of live birth success for a twin pregnancy with a 39-year-old woman who is using embryos that have undergone genetic testing is 60%, with the expectation that 10% will result in loss.
Q: What is the egg supply and health of the average 39-year-old woman?
A: In order to identify genetically normal embryos for a woman at this age, we typically need to test embryos for genetic health until we have 2-3 viable embryos. This may take multiple IVF cycles to achieve.
Q: What are the odds that two embryos could create triplets?
A: Just 1% – the odds are very low!
Q: How can Paris sharing her story help others?
A: Awareness is ALWAYS needed so that patients with infertility don’t feel alone. Every story breaks down barriers for the infertility community and helps to remove the sense of shame felt by many infertility patients.
Medical contribution by Jennifer Hirshfeld-Cytron, M.D.
Dr. Hirshfeld-Cytron is board certified in both Obstetrics and Gynecology and Reproductive Endocrinology and Infertility and has been practicing medicine since 2004. She completed her Obstetrics and Gynecology residency at the University of Chicago, and then completed her three-year fellowship in Reproductive Endocrinology and Infertility at Northwestern.