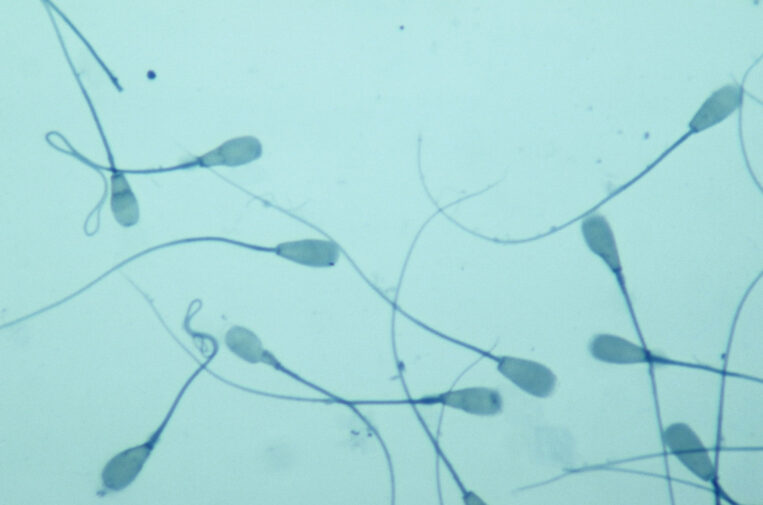
The production of sperm by the Sertoli cells within the seminiferous tubules of the testis, referred to as “spermatogenesis”, is a complicated process. Spermatogenesis is highly dependent on testosterone production by the Leydig cells of the testis, as well as many other testicular and pituitary hormone interactions.
The development of each spermatozoa requires 2-3 months for completion. For that reason, if a man should require medical treatment to improve spermatogenesis, he must wait 2-3 months before any therapeutic effects may be seen.
In order to better understand the anatomy of the testis, imagine the seminiferous tubules to be tiny spaghetti noodles pressed together. Within the interior of these “noodles” sperm production takes place with sperm development within the Sertoli cells that surround the sperm cells, nurturing them with nutrients and chemicals that direct the complicated production of sperm. Between the “noodles” lay the Leydig cells that make testosterone.
After production of the sperm in the testis, they mature in the epididymis, a small structure attached to the testis. I often describe its positioning as the “acorn cap” on the “acorn”, with the “acorn” being the testicle. It sits on top of the testicle and then drapes along the outside edge. From the epididymis, sperm travel through the vas deferens, finally emptying into the ejaculatory ducts located within the prostate, where sperm mix with seminal fluid from the prostate and the seminal vesicles.
Azoospermia is a condition where no sperm are found in the ejaculated semen. In cases with low ejaculatory volume (less than 1 ml), retrograde ejaculation should always be ruled out. This is done by having you urinate into a specimen cup after ejaculation. Azoospermia may be caused by obstruction of the epididymis or vas deferens (“obstructive azoospermia”- OA) or there may be problems associated with defective production of sperm (“non-obstructive azoospermia”- NOA). A Urologist/Andrologist can usually distinguish between the two by measuring testis size and the FSH hormone levels. A biopsy of the testicle is rarely needed.
Obstructive azoospermia may be associated with congenital defects such as congenital bilateral absence of the vas deferens (CBAVD), often associated with cystic fibrosis (or even the cystic fibrosis carrier state) or maybe due to injury, infection, or elective vasectomy. If the obstructive azoospermia can be corrected surgically, this is often a more cost-effective option. If surgical repair or reconstruction is not possible or is ultimately not successful, then sperm must be extracted from either the testis or epididymis.
Extracted sperm can then be utilized with In Vitro Fertilization (IVF) and intracytoplasmic sperm injection (ICSI). For obstructive azoospermia, MESA, (microscopic epididymal sperm aspiration) or PESA (percutaneous epididymal sperm aspiration) is one option, though this option would prevent the possibility of future reconstruction. Of the two, MESA will often yield a better sample. A TESE (testicular sperm extraction) is often utilized as a means of obtaining a greater amount of sperm in hopes of avoiding the need for any additional future procedures if additional IVF cycles are needed. Testicular sperm has less motility than epididymal sperm (only about 5% of testicular sperm is motile), but most IVF labs are well-equipped to utilize either type of sample. Motility is not necessary for ICSI.
Non-obstructive azoospermia also may be congenital or it can be acquired later in life due to injury, infection, or other harm to the testicle. Some of these causes can be medications (chemotherapy for example) or anatomical abnormalities (varicocele). In some cases, pre-treatment with medications such as clomiphene citrate to stimulate spermatogenesis may help as adjunctive therapy prior to sperm retrieval. Data has demonstrated that for individuals with abnormal hormonal profiles, there is an increased success rate of surgical sperm retrieval when clomiphene citrate is used prior.
In cases of severe oligospermia, (sperm count less than 5 million/ml) and especially with azoospermia, genetic screening may be very helpful. For example, the chance of finding sperm in men with NOA is essentially 0% if they have a genetic microdeletion of the Y chromosome at the AZF A or B locus. On the other hand, NOA cases caused by mumps, torsion, cryptorchidism and idiopathic causes may be associated with a 40-60% chance of finding sperm. In cases of NOA, sperm are generally extracted from the testes by microTESE (microdissection testicular sperm extraction).
MicroTESE is often successful due to the concept that the seminiferous tubules containing sperm are “thicker” or “plumper” than those that don’t contain sperm. General anesthesia and 25 times magnification are required given that these tubules are incredibly thin. Another technique involves office FNA mapping (fine needle aspiration) followed then by directed TESE. Data on the benefits of mapping remains inconclusive, so FNA mapping is not a universally accepted and utilized method at this time.
In cases of OA and NOA involving both epididymal and testicular sperm extraction, the IVF/ICSI pregnancy rates appear to be essentially the same with fresh or frozen sperm. Since IVF/ICSI is far less than 100% successful, it behooves the reproductive urologist/andrologist to utilize sperm retrieval techniques that are reliable, associated with low morbidity, but also have the potential to harvest sufficient sperm in order to enable cryopreservation for future IVF/ICSI attempts should they be needed. With the equivocal outcomes using fresh versus frozen sperm, extraction is often done first to assure that surgical sperm retrieval is successful prior to the female partner undergoing her ovarian stimulation and egg retrieval procedure.
Summary
In obstructive and non-obstructive azoospermia, the urologist/andrologist can use many different methods for extracting sperm from the testis and/or epididymis including open surgical extraction, microsurgery, as well as needle aspiration. As stated above, with obstructive azoospermia, since larger numbers of sperm are present, more choices are possible. However, with non-obstructive azoospermia, in order to obtain enough sperm from the testis, open microsurgery is the established gold standard.
Medical contribution by Samuel Ohlander, M.D.
Dr. Samuel Ohlander is committed to building a trusting relationship with his patients by providing honest, compassionate, and collaborative care. He is board certified in Urology and specializes in male infertility, fertility preservation, low testosterone, vasectomies, and microsurgical vasectomy reversals.